As a nurse who works in the emergency department, I have seen it all.
People at their worst and sometimes at their best.
To provide compassionate care in this challenging setting, it takes two, the nurse and the emergency department care provider.
I have been blessed to work with an exceptional and experienced ED physician by the name of David Peterson. He is compassionate but also practical.
Those who work in stressful settings such as emergency care, are known to develop a dry sense of humor to keep ones sanity when everything seems to be falling apart.
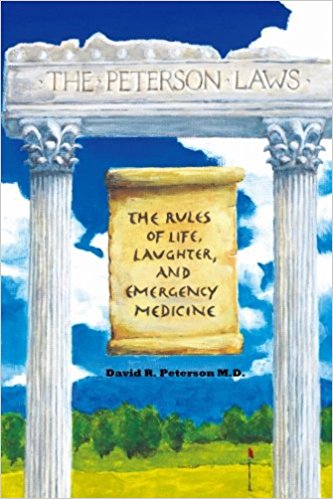
Dr. David Peterson has written a book The Peterson Laws that contain 71 practice based principles gleaned from over 25 years of clinical practice.
Though written from a physician’s lens of practice, it can also provide insights that can help prepare nurses with insights from real-world clinical practice.
Law #71:Is your medical patient also a “psych” patient?
Dr. Dave has laws titled, “You can’t teach common sense”, “Never try to pacify someone at the height of his or her rage”, and “All bleeding eventually stops”.
Today, I want to share and highlight law #71. It is titled how to determine if your patient is a psychiatric patient.
From a nursing perspective, I would filter this law with the importance of “avoiding assumptions” or making judgments about a patient.
Consider the following insights as “red flags” that need to be considered as you gather additional assessment data to cluster and make a clinical judgment.
He writes:
I have noticed the connection between multiple allergies and psychiatric conditions right away as a resident, and then started to make a conscious note each time I encountered this. Knowing that a person may be a psychiatric patient can give you insight into the pathology of their current complaint.
Sometimes psychiatric patients have somatization, which is a physical symptom due to a psychological condition.
There are other more subtle conditions that can affect the evaluation of your patient. Narcissism, obsessive-compulsive disorder, and general hypochondria can impact how you examine and diagnose a patient.
Narcissism also plays a role in patient behaviors as well. All people want to be “special”. Some just go out of their way to show it.
Clinical Red Flags
To determine if your patient who is not on a mental health unit may have a mental illness, psychological condition, or is “special” if any of the following are present you may want to consider this possibility.
1. Three or more allergies in different drug classes
An allergy must not just be a side effect that makes you vomit. Some people say, “I’m allergic to all antibiotics” which of course makes no sense.
Antibiotics have wildly different chemical structures and God is not mean enough to make someone allergic to all of these wonder drugs.
A patient who has an extensive list of allergies to drugs, consider this a clinical red flag that they either have side effects which are NOT allergies, or may be a psychiatric patient.
2. Allergic to any psychiatric medication
This should be self-explanatory I hope. If you are allergic to a psychiatric medication, you have some form of mental illness if that is the reason you received the medication.
3. Allergic to non-allergenic meds such as cortisone, diphenhydramine and other antihistamines
This really puts you into the “special” category when you can’t take a medication that treats allergic reactions because you’re allergic to it.
Furthermore how can you be allergic to cortisone? It’s something your own adrenal glands create in your body and you can’t live without it.
4. Three or more unrelated chief complaints
Your body just doesn’t create three separate emergencies at the same time. Nobody has that much bad luck. Therefore having three completely unrelated chief complaints, not secondary complaints but chief complaints indicate that the mind may be at work manufacturing symptoms.
A person having a heart attack can have chest pain, nausea, and sweating. Although seemingly unrelated, they are part of a symptom complex, so they count as one.
A good example of this principle would be a patient saying, “I am depressed and suicidal. I also have new sharp lower back pain, and I also have a nail in my leg from a nail gun.”
5. Anyone who says, that’s a fever for me
When I tell the patient that their temperature is normal at 98.5 degrees, but they came in for a fever and the patient says, “No I usually run 97°, that’s a fever for me!”
It is possible that humans vary slightly in their core temperature. But not over a degree and a half! What species are you then?
Mammals have similar cell structures and their innards work at 98.6°. Did your mom Mary a reptile? I’m sorry, but no you aren’t special, your current temperature of 98.5 is normal. Even for you.
No you do not need an antibiotic. Good luck convincing them of this. You can’t. If you could, they wouldn’t be special anymore. And they need to be special.
In Closing
The perspectives of Dr. Dave are gleaned from the crucible of decades of clinical practice.
They are in no way meant to be prejudicial, but observations based on patterns that he has observed in this challenging setting.
Though you may not agree with everything he writes, consider and do not quickly discount these reflections.
If you are in need of tongue-in-cheek humor as well as pearls to strengthen your practice, The Peterson Laws can help any health care worker be better prepared for real-world clinical practice!.
Want More?
Simply click the image below for more information and how to purchase from Amazon.
Keith Rischer – PhD, RN, CEN
As a nurse with over 35 years of experience who remained in practice as an educator, I’ve witnessed the gap between how nursing is taught and how it is practiced, and I decided to do something about it! Read more…
The Ultimate Solution to Develop Clinical Judgment Skills
KeithRN’s Think Like a Nurse Membership
Access exclusive active learning resources for faculty and students, including KeithRN Case Studies, making it your go-to resource.




