Whenever I ask educators to share their greatest struggle, it revolves around the difficulty to help students put the clinical puzzle together and think more like a nurse.
Can you identify with these struggles educators have in the clinical setting…
- “Getting students to connect the dots between labs, diagnosis, patho, meds, and nursing interventions”
- “Getting students to put the pieces of the clinical puzzle together”
- “Getting students to think like a nurse with clinical paperwork that is not busywork”
If this is also your lived reality, you are not alone. These are universal struggles that clinical educators encounter.
The greater question is:
HOW can educators move the ball forward to OVERCOME this struggle and help students put the clinical puzzle together to think more like a nurse?
To put the pieces of the clinical puzzle together, students need to IDENTIFY and RECOGNIZE six clinical relationships.
Recognizing RELATIONSHIPS
Pattern recognition is the first step of intuitive clinical judgment making, that guides advanced nurse thinking. It is the ability of the nurse to recognize RELATIONSHIPS of patterned patient responses (Benner & Tanner, 1987).
Recognizing clinical relationships is another “way of thinking” (Benner, Sutphen, Leonard, & Day, 2010, p. 84) that can help students think more like a nurse.
When clinical relationships are recognized and identified by the student, clinical data collected begins to “fit” and the patient puzzle begins to “fit” and come together.
As I reflected upon my 35 years of clinical practice, I recognized SIX distinct RELATIONSHIPS that I used intuituvely as an experienced nurse to put the puzzle together, but recognizing these RELATIONSHIPS is a nurse thinking skill that is not taught in textbooks, yet is required to think more like a nurse.
Strengthen the thinking of your students by integrating these six clinical relationships, especially in the clinical setting:
SIX Clinical Relationships
- RELATIONSHIP between RELEVANT present problem data and the primary medical problem
- RELATIONSHIP of the past medical history and current medications
- RELATIONSHIP between RELEVANT clinical data and the primary problem
- RELATIONSHIP between the primary medical problem and nursing priority
- RELATIONSHIP between the primary care provider’s orders and primary problem
- RELATIONSHIP between diseases in PMH that may have contributed to the development of the current problem
These relationships can also be used as QUESTIONS to ask students in the clinical setting to identify these “puzzle pieces” with their patient so they can begin to put it together.
To strengthen your understanding of how these clinical relationships can be used to strengthen your students thinking, let’s contextualize these relationships with the same scenario we used in last week’s blog on sepsis.
Sepsis Case Study
Jean Kelly is an 82-year-old woman who has been feeling more fatigued the last three days and has had a fever the last twenty-four hours. She reports a painful, burning sensation when she urinates as well as frequency of urination the last week. Her daughter became concerned and brought her to the emergency department (ED) when she did not know what day it was. She is mentally alert with no history of confusion. While taking her bath today, she was weak and unable to get out of the tub and used her personal life alert button to call for medical assistance.
Clinical RELATIONSHIP #1
What is the RELATIONSHIP between RELEVANT present problem data and the primary medical problem?
To recognize this clinical relationship, students must have a strong “wall” built of applied pathophysiology.
The pathophysiology of sepsis/SIRS must be DEEPLY understood so students can identify what clinical data is RELEVANT and how it is RELATED to the patho of sepsis.
Past Medical History
- Diabetes type 2
- Hyperlipidemia
- Hypertension (HTN)
- Gout
Home Medications
- Allopurinol 100 mg PO bid
- ASA 81 mg PO daily
- Pioglitazone 15 mg PO daily
- Simvastatin 20 mg PO daily
- Metoprolol 25 mg PO bid
- Lisinopril 10 mg PO daily
- Furosemide 20 mg PO daily
- Potassium chloride 20 mEq PO daily
Clinical RELATIONSHIP #2
What is the RELATIONSHIP of the past medical history and current medications?
This is the most basic clinical relationship that fundamental students can be guided to recognize.
To identify the clinical relationship of what current medications are treating past medical problems, the nurse must know not only what the medication is for, but based on the patient’s history, why is he receiving it.
The nurse colects the following data:
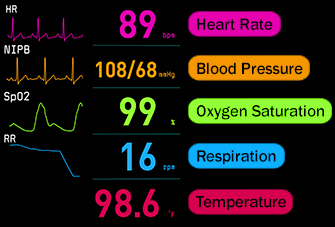
| T: 101.8 F/38.8 C (oral) |
| P: 110 (regular) |
| R: 24 (regular) |
| BP: 102/50 |
| O2 sat: 98% room air |
Pain Scale:
| Provoking/Palliative: | Nothing/Nothing |
| Quality: | Ache |
| Region/Radiation: | Right flank |
| Severity: | 5/10 |
| Timing: | Continuous |
The nurse recognizes the need to validate his/her concern of fluid volume deficit and performs a set of orthostatic VS and obtains the following:
| Position: | HR: | BP: |
| Supine | 110 | 102/50 |
| Standing | 132 | 92/42 |
| Current Assessment: | |
| GENERAL APPEARANCE: | Resting comfortably, appears in no acute distress |
| RESP: | Breath sounds clear with equal aeration bilaterally, nonlabored respiratory effort |
| CARDIAC: | Pink, warm and dry, no edema, heart sounds regular-S1S2, pulses strong, equal with palpation at radial/pedal/post-tibial landmarks |
| NEURO: | Alert and oriented x2-is not consistently oriented to date and place, c/o dizziness when she sits up |
| GI: | Abdomen soft/nontender, bowel sounds audible per auscultation in all four quadrants |
| GU: | Dysuria and frequency of urination persists, right flank tenderness to gentle palpation |
| SKIN: | Skin integrity intact, lips dry, oral mucosa tacky dry |
Clinical RELATIONSHIP #3
What is the RELATIONSHIP between RELEVANT clinical data and the primary problem?
To recognize this clinical relationship, students must be able to identify the most important clinical data and relate it to the primary medical problem.
Relevant clinical data would include physical assessment findings, vital signs, and laboratory values.
How Did You Do?
Because the questions are open ended, were you able to identify and recognize these clinical RELATIONSHIPS?
I have developed a total of 24 med/surg and specialty topics of Clinical Reasoning 1-2-3 that you can put to immediate use and have students practice this is essential component of clinical reasoning in the safety of your classroom or clinical post-conference setting.
How to Use
This case study is case study #2 in my new series Clinical Reasoning 1-2-3 that are THREE short, sequential case studies that are only 2-3 pages and can be completed in about 15-20 minutes start to finish.
This makes it possible to easily integrate as an active learning tool after teaching on a topic related to this case study.
If you are teaching in the clinical setting, during post-conference, once reflection of the clinical day has taken place, finish strong and use this case study for the last 15 minutes to practice recognizing RELATIONSHIPS with a topic relevant to your clinical setting.
How to Save $10 on this Sepsis Case Study
Put this case study to work in your program immediately and save $10, but only through Sunday, February 5th!
Click this link for SEPSIS Clinical Reasoning 1-2-3, and all THREE case studies on this topic. Bundle includes blank student version and fully developed answer key!
In Closing
In order to clinically reason and think more like a nurse, students must be able to recognize clinical RELATIONSHIPS.
Make each of these clinical relationships a question and use these questions in your next clinical or post-conference to strengthen student clinical thinking.
By guiding your students to identify and then recognize these clinical relationships, you will be well on your way to helping your students put the clinical puzzle together and help them think more like a nurse!
What do you think?
How have you helped students put the clinical puzzle/picture together and strengthen their ability to think more like a nurse?
Comment below and let the conversation begin!
Want More? Get Clinical Reasoning 1-2-3!
PRACTICE the nurse thinking skill of clinical reasoning with Clinical Reasoning 1-2-3 case studies . Highlights of each case study include:
Case Study/Step #1: Recognize RELEVANCE and PRIORITIES
Emphasizes the essence of clinical reasoning and the importance of identifying and interpreting RELEVANT clinical data of the initial scenario, VS, assessment, and labs to establish the correct nursing priority.
Case Study/STEP #2: Recognize Clinical RELATIONSHIPS.
Builds on the essence of clinical reasoning by emphasizing the nurse thinking skill of recognizing clinical relationships. These relationships include in part, the RELATIONSHIP of the past medical history and current medications, the RELATIONSHIP between RELEVANT present problem data and the primary medical problem and four more that students must know!
Case Study/STEP #3: Care Like a Nurse by Providing Holistic Care.
Emphasizes the importance of holistic care and the relevance of the “art” of nursing by addressing psychosocial priorities and how caring, empathy, engagement, therapeutic communication can be utilized to provide holistic care.
References
- Benner, P. & Tanner, C. (1987). Clinical judgment: How expert nurses use intuition. American Journal of Nursing, 87(1), 23-31.
- Benner, P., Sutphen, M., Leonard, V., & Day, L. (2010). Educating nurses: A call for radical transformation. San Francisco, CA: Jossey-Bass.
Keith Rischer – PhD, RN, CEN
As a nurse with over 35 years of experience who remained in practice as an educator, I’ve witnessed the gap between how nursing is taught and how it is practiced, and I decided to do something about it! Read more…
The Ultimate Solution to Develop Clinical Judgment Skills
KeithRN’s Think Like a Nurse Membership
Access exclusive active learning resources for faculty and students, including KeithRN Case Studies, making it your go-to resource.