Even though I have been in practice for over 30 years, I continue to use mnemonics as a tool to help me remember each step of a complete pain assessment when a patient comes into the emergency department. “WILDA” is not a woman, but an mnemonic that accomplishes this needed objective for me!
As novice nurses, students will value and appreciate any practical mnemonic that they can use to ensure that they too did not miss a step in their pain assessment, head to toe assessment or even cardiac auscultation landmarks on their patients.
In todays blog, I will share the mnemonics that I find most useful in my clinical practice. But I will save the best for last…a mnemonic for a complete head-to-toe assessment developed by Cynthia Stoerzbach, RN, MS, CNE, a nurse educator at Carl Sandberg College, Galesburg, Illinois that was sent to me to include as an “educational pearl” for my new book coming later this year Teaching to Transform, that I want to share with all of you today.
Some mnemonics are used to pass a difficult test, but are quickly forgotten or have no application to clinical practice. Am I the only one who used the mnemonic “on old Olympus tiny top a Finn and German viewed some hops” to remember the 12 cranial nerves for A&P?
The following are mnemonics that can help your students remember what is most important in the clinical setting:
W-I-L-D-A (Pain)
Since pain is such a common assessment as well an important response that must be completely and concisely documented, I have two mnemonics that I use to help me accomplish these needed objectives:
- W-Words…that describe the pain
- I-Intensity…scale of 1 to 10
- L-Location…specific location of pain
- D-Duration..how long has the pain lasted/intermittent or continuous
- A-Aggreviating/Alleviating factors…what makes the pain worse or what makes the pain better
P-Q-R-S-T (Pain)
- P-Provoke/Palliative…what makes the pain worse or what makes the pain better
- Q-Quality…words that describe the pain
- R-Radiation…does the pain radiate to other parts of the body
- S-Severity…scale of 1 to 10
- T-Timing…how long has the pain lasted/intermittent or continuous
In addition to using these mnemonics to perform any pain assessment, be sure that your students step back and ask the following question for any patient complaint of pain:
Is this pain EXPECTED or UNEXPECTED for my patient based on the reason they are in the clinical setting?
Incisional pain that is localized to the abdomen that is severe on day of surgery of day #1 after surgery is obviously expected. Abdominal pain 3-4 days later that is generalized, severe, and combined with assessment findings of firm, distended abdomen, nausea & vomiting is NOT expected and could be an ileus or bowel obstruction that must be recognized as being clinically significant to the nurse.
See my blog post “Jason is Still Out There” for more information on the importance of nurse vigilance and looking for the worst possible/most likely complication.
A-P-T-M (Cardiac Landmarks)
Students MUST know the location and physiologic landmarks of the four valves: aortic, pulmonic, tricuspid, and mitral. It was not uncommon for my advanced students to struggle with correct identification of these landmarks. This is important because some patients have valvular disease or have had valve surgery and students must know the location of that valve and listen carefully for any murmurs or adventitious sounds.
Though I am not an advocate of the theory of evolution, the mnemonic APe To Man will help students remember the correct sequence of a cardiac valvular assessment:
- Aortic valve is second intercostal to the RIGHT of the sternum. The manubrium is the “bump” on the top end of the sternum that is the landmark for the second intercostal space.
- Pulmonic valve is also second intercostal across the sternum on the LEFT side.
- Tricuspid valve is fourth to fifth intercostal on the LEFT side of the sternum. This level is also consistent with the nipple line of men, and is the lower third of the sternum to visualize for women.
- Mitral valve is the same intercostal level, just slide the stethoscope over to LEFT mid-clavicular. On a male this is typically right at the left nipple. This is also the location for an apical pulse.
I teach my students to be considerate of women when auscultating the tricuspid and mitral valves which are over the left breast, auscultate ABOVE the breast so it is not as intrusive by auscultating BELOW the breast.
M-W (Head-to-Toe Assessment)
The use of the M-W acronym provides the student nurse with a method to recall the basic physical assessment data of the patient and the ability to transfer this information to various types of documentation systems. The mnemonic that Cynthia developed provides a “sticky ” method to recall information and prevent omission of patient assessment data , affecting the plan of care.
M-Musculoskeletal: General mobility and strength of extremities, general ROM, strength of hand grasps
N-Neuro: Response to stimuli, alert and oriented to person, place, time and situation
O-Oh my: What has happened to you lately: details (location, type, size, etc.) of tubes, drains, IV sites, wounds, sutures, staples, dressings
P-Pain: Location, duration, intensity, related signs of pain and recall of most recent medication with effectiveness
Q-Cardiac: Quality of heart tones, rhythm, amplitude, radial and pedal pulses bilaterally, presence of edema
R-Respiratory: Depth, auscultation of upper/ lower, anterior and posterior lung fields, nail bed and lip color, cap refill, presence of cough
S-Skin: General skin temp and moisture, assess overall skin integrity and pressure points
T-Tummy: Bowel sounds, palpation of abdomen, nausea or level of appetite, ask about most recent BM with characteristics
U-Urinary: Assess urinary catheter or ask about last urination, color, clarity, amount and ease of elimination
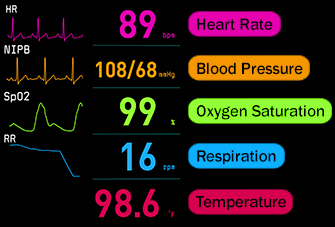
V -Vital signs: Temp (assessment device utilized), B/P with position, pulse rate (identify if apical or radial or A/R) respiratory rate, pulse ox and use of oxygen with delivery of type and percentage of oxygen
W -We will be Safe: Top side rails up, call light in reach, phone at bedside, personal alarm on, etc.
In Closing
Though some mnemonics are in textbooks, I know that nurse educators are inherently creative and many of you are aware of other mnemonics or have created your own. Remember that the neuronal “ruts” of novice nursing students are not well established and require practice to establish. Therefore do all that you can to help them to transfer learning to the clinical setting where it matters most using easy to remember mnemonics!
Comment Question:
Have you created or know of a mnemonic has been helpful to promote the learning of your students?
If so please comment & share below!
Keith Rischer – PhD, RN, CEN
As a nurse with over 35 years of experience who remained in practice as an educator, I’ve witnessed the gap between how nursing is taught and how it is practiced, and I decided to do something about it! Read more…
The Ultimate Solution to Develop Clinical Judgment Skills
KeithRN’s Think Like a Nurse Membership
Access exclusive active learning resources for faculty and students, including KeithRN Case Studies, making it your go-to resource.